May 5, 2023
Measuring the Health Benefits of Energy Efficiency Programs
More work is needed to help programs succeed in both saving energy and protecting people’s health.
By: Ronald Denson Jr. and Sara Hayes
Scores of programs in the United States and abroad have the goal of saving energy and improving human health. Programs commonly address exposure to mold, lead, and radon as well as malfunctioning or inefficient appliances, which are potential sources of fire and CO. Some programs take measures to eliminate pests, such as cockroaches and rats, which can carry disease and expose people to allergens. The Next Nexus report (Denson Jr. and Hayes, 2018) highlights several of these programs, describes common practices, and includes case studies.
Mechanisms for tracking the impact of these programs on health are not as established as the methods used to evaluate, measure, and verify energy savings realized by these programs. Many programs that aim to improve health do not report health results related to their work. This is problematic, because evidence-based practice built on research findings and basic science is needed to demonstrate a program’s success. Lacking evidence-based practice, it can be incredibly difficult, if not impossible, to determine whether a particular measure or set of measures is truly improving the health of the individual receiving an intervention.
When asked, “Does the program include documented and verified health outcomes?” 10 of the 49 programs described in the Nexus report said, “Yes.” However, only 3 of the 10 were able to share those results. The report offered various reasons to explain why so few programs submitted health outcomes. Some programs did not have the information when they submitted their results and indicated in follow-up correspondence that they would submit it later. Others recorded health outcome data for internal use only and were unable to make their findings public. Some programs did conduct preintervention surveys, audits, or assessments, but did not conduct postintervention testing, limiting the usefulness of the baseline data they collected.
Initial Audit or Baseline Assessment
Initial assessments can be used to establish a baseline to determine whether occupants’ health has improved once a home intervention is complete. Often called home health assessments or environmental health assessments, these evaluations may consider air quality, exposure to mold, extreme temperature swings, the presence of pests, and more. As we said earlier, only 10 of the 49 respondents reported that their programs document and verify health outcomes. Of those, 9 conducted some form of preintervention environmental health assessment.
While these programs use different forms of baseline assessment, there are some common elements among them. Some programs assess the health of household members by tracking the number of times they visit the emergency department; some evaluate the environment to assess pre- and postintervention air quality; and some track symptoms related to specific medical conditions, such as asthma or chronic obstructive pulmonary disease (COPD).
Postintervention Assessment
Most programs that reported tracking health outcomes used postintervention assessments, but the type of data collected and the methods used vary. As with the baseline assessments, some programs test the environment, measuring things like radon and particulate matter in the home environment. Other programs track hospitalizations or medical interventions for building occupants, particularly outcomes related to asthma. Some programs also measure how their activities might affect the outside environment, reporting things like gallons of water saved and tons of carbon emissions avoided.
Case Studies
Here are four standout programs that do both an initial audit and a postintervention assessment.
The Grassroots Green Homes Program
GGH was founded by Conservation Consultants Incorporated (CCI), in Pittsburgh, Pennsylvania. Since its inception in 2016, this neighborhood-driven program has reached more than 600 residents. Now completing its second neighborhood engagement, GGH engages program participants on many levels, ranging from affordability to health. The program works in collaboration with local government agencies and community-based organizations, including local electric and gas utility companies, a healthy homes nonprofit, and the state weatherization assistance program (WAP). GGH is funded primarily by private foundations. Focusing largely on single-family homes, the program has three components—Weatherization Plus services, Energy Coaching, and the Energy Efficiency Challenge.
The Grassroots Green Homes program is free of charge and open to both homeowners and renters in select—mostly low-income—Pittsburgh neighborhoods. GGH uses door-to-door outreach, presentations at community events, and flyers to advertise its offerings. Energy Coaches are volunteers trained to become neighborhood resources. Interested individuals must complete a survey detailing their personal demographics, the condition of their home, and their behaviors and perceptions related to energy efficiency. They must also complete a Utility Authorization Form, which allows the utility companies to release a participant’s usage information. This helps CCI determine whether and how savings are achieved, and to accurately assess pre- and post-intervention energy outcomes.
The Energy Efficiency Challenge is the program’s main component. It consists of 12 monthly toolkits. One example includes items such as:
- a monthly survey to help program administrators track intervention adoption status, ease of use, and intention to continue use;
- a combination thermometer/hygrometer (used to measure temperature and humidity, respectively);
- instructions on how to check humidity levels and check for mold and mildew;
- guidance on using kitchen and bathroom vents to reduce indoor humidity; and
- a program newsletter with information on supplemental non-GGH resources.
The Weatherization Plus component is free to a small subset of homes in the Energy Efficiency Challenge and includes a home health assessment, an energy audit, air sealing, insulation, weather-stripping, and energy-efficient appliance upgrades, as well as testing and mitigation—where appropriate—of mold, lead, CO, and radon. GGH recruits community volunteers to be Energy Coaches. These Energy Coaches are trained in home health and energy efficiency topics in order to share that information with their neighbors.
Once the intervention is complete, the qualitative data from the surveys is coupled with the quantitative data from the utility companies to establish what, if any, changes in comfort, health, and energy use have occurred since the program was implemented. Some of the participating households opted into an additional indoor air quality (IAQ) study measuring particulate matter pre- and post-intervention.
Preliminary data demonstrated significant reductions in radon where mitigation systems were installed and reductions in mold where moisture issues were addressed.
The Bronx Healthy Buildings Program
Established in 2015, the Bronx Healthy Buildings program has served more than 100 multifamily households in the Bronx, New York. Using data analysis, program administrators, together with their program partners, target residential buildings with high incidences of asthma-related emergency room visits and hospital admissions associated with the built environment. The analysis consists of a data overlay that contains information from several sources, including asthma patient records from the Montefiore Medical Center’s electronic medical records system; heat complaints and housing violations from the NYC Department of Housing Preservation and Development; building owners on the wait list for the Northwest Bronx Community and Clergy Coalition (NWBCCC) WAP; and buildings that are required by New York law to start using renewable heating oil.
The Bronx Healthy Buildings program is administered primarily by the NWBCCC. Montefiore Medical Center and the New York City Department of Health and Mental Hygiene are the cofacilitators; other program partners (among the 14 total) are the Emerald Cities Collaborative, New York Lawyers for the Public Interest, and New York City Councilman Ritchie Torres. The Bronx Healthy Buildings program is funded by the BUILD Health Challenge—a consortium of organizations that aim to encourage communities “to build meaningful partnerships among hospitals and health systems, community-based organizations, their local health department, and other organizations to improve the overall health of local residents.” The program also receives funding from the Bronx Partners for Healthy Communities and DOE’s WAP.
Program representatives engage the targeted residents to determine their interest in the intervention. They also foster nonadversarial relationships between residents and property owners to ensure collaboration as the program proceeds. Once targeted households express interest, Bronx Healthy Buildings staff members perform energy audits, analyze fuel usage, and conduct home visits to perform health and environmental assessments. Energy efficiency measures that are also meant to improve occupant health include replacing windows; air sealing; and insulating pipes, roofs, sidewalls, and radiator vents.
The health workers give hypoallergenic pillowcases and mattresses to participants with asthma and connect them with smoking cessation resources. They also provide other safety and health measures, including smoke and CO detectors and mold remediation. To deal with pests, they seal holes, eliminate sources of food and water, manage garbage, and apply pesticides as necessary. Finally, health workers provide informational materials on IAQ hazards, mold, and lead, as well as on energy saving and water conservation. They also offer training on the social determinants of health, leadership, and community organizing.
To track the program’s effectiveness at reducing utility bills and morbidity related to chronic illnesses such as asthma, administrators conduct three different evaluations before and after work is performed. First, they compare health care cost and usage before and after the intervention. Second, they examine self-reported data from participants on such topics as general health, respiratory health, education, the home’s condition, and the residents’ sense of urgency related to their health and environment. Third, they track electricity, oil, natural-gas, and water usage.
This program has served hundreds of Bronx residents, helping them save up to 18% and 20% on their gas and electric bills, respectively. This program model has reduced allergens and other asthma triggers, resulting in reductions in avoidable hospital admissions (91%), avoidable emergency department visits (65%), and avoidable school absenteeism (65%) caused by respiratory illness. These results were taken from information submitted on nomination forms detailed in the Next Nexus report. The data used to determine these outcomes are not publicly available.
The Healthy Homes Initiative
Rutland Regional Medical Center (RRMC) and local home improvement organization NeighborWorks of Western Vermont (NWWVT) initiated the Healthy Homes Initiative as a collaborative effort in 2016. The program is funded by RRMC’s Bowse Trust, which was created to support community-based projects that improve health.
Recognizing that healing continues long after a patient has left the hospital, this program uses RRMC’s and NWWVT’s respective expertise to address the health and safety problems in patient’s homes for low-to-middle-income Rutland County residents. Low to middle income is defined by this program as up to 120% of area median income.
The program is not actively marketed. Instead, patients are enrolled in the program after receiving an electronic referral from the hospital, primary care, or medical specialist’s office. Priority assistance goes to patients who are fall risks; who have accessibility problems, asthma, or COPD; and who would benefit from home improvements that would improve their health. Program participants are given a grant of up to $6,000, which is matched by a loan, if needed, to have the necessary work done.
Once the patient receives the referral, a steering committee triages each case and determines each participant’s health and financial needs. Next, a NWWVT staff member schedules a meeting with the patient to discuss available grant and loan opportunities and to set up a home audit to assess which needed repairs are high priority. Finally, a NWWVT Home Repair team and crew of contractors begin necessary renovations. Implemented measures include air sealing, roof repair, pre and post energy audits, carpet replacement or removal, radon and CO monitoring, HVAC repair or replacement, and installing ramps or widening doorways.
RRMC staff track the number of emergency department visits and admissions to their facility for each patient who has participated in this joint program pre- and postintervention. While all enrolled-patient health outcomes are recorded, specific data on the health impacts of the program are not currently publicly available.
The Green & Healthy Homes Initiative Asthma Reduction Program
Created in 2008, the GHHI program model uses a holistic approach to help thousands of households in more than 50 GHHI sites and innovative healthcare financing sites nationwide. GHHI offers participants in either single or multifamily homes multiple health and energy services through an integrated process that produces comprehensive interventions.
With strong support from HUD, the Centers for Disease Control and Prevention (CDC), DOE, the National Environmental Health Association, and local and national foundations, the GHHI integrated model was launched nationally in 2010 at 14 sites across the country. The Council on Foundations, HUD, CDC, and the White House Office of Recovery commissioned GHHI to take a national leadership role on issues involving healthy homes, lead hazard reduction, weatherization, and energy efficiency.
GHHI-supported housing programs serve primarily low-income households. They emphasize homes that are occupied by children, pregnant women, and seniors and that need lead hazard and asthma trigger reduction, household injury prevention measures, and weatherization or energy efficiency interventions. GHHI housing programs serve families living in areas with some of the nation’s highest rates of negative health quality indicators. These include housing and health code violations, fires, deteriorated housing stock, childhood asthma emergency room visits and hospitalizations, childhood lead poisoning, and household injuries. GHHI replaces stand-alone housing intervention programs with an integrated, whole-house approach. It works nationally to advance innovation in the field by creating systems change, documenting cost-benefit analysis, educating policy makers, building organizational capacity at the state and local level, and creating new financing pathways such as Pay for Success, as well as health care and philanthropic investment strategies.
Based at GHHI’s site in Baltimore, Maryland, GHHI’s Asthma Reduction program targets households with children ages 2–14 who have asthma. Participants are referred to GHHI by local community partners and medical providers and are enrolled in the program through GHHI’s client intake coordinator, who confirms client eligibility.
Once the client is enrolled, the program begins with an initial phone interview to gather information for baseline data. This is followed by an in-home assessment consisting of a health evaluation by GHHI’s environmental health educator. The health assessment is conducted with the client to assess any conditions that are contributing to negative health outcomes. GHHI’s environmental assessor performs an environmental assessment and energy audit. The environmental assessment identifies asthma triggers, household injury risks, and other home-based environmental health hazards such as mold, lead, radon, and asbestos. The results of these assessments are used to devise a plan to assist the client with asthma trigger reduction and other objectives. Following the development of a comprehensive plan, program managers coordinate the various braided funding sources and connect participants with GHHI’s in-house crew or other appropriate professionals who can perform the suggested work in the home.
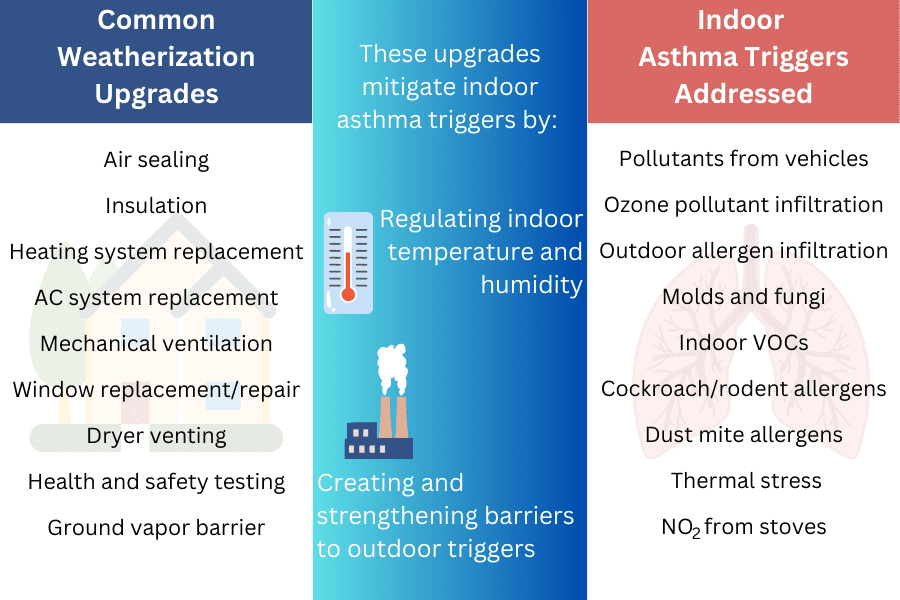
GHHI uses energy efficiency and weatherization measures combined with lead hazard reduction, healthy homes interventions (asthma trigger reduction, injury prevention, and other hazard reductions), housing rehabilitation, and resident education interventions to achieve its results.
Participants receive in-home resident training on asthma management and behavioral change to help reduce asthma triggers and household injury risks, as well as guidance on energy conservation to help reduce energy consumption and costs. Asthma-specific intervention measures include integrated pest management; mold remediation; mattress and pillow cover installation; carpet removal; kitchen, bathroom, and dryer ventilation; and installation of an air-filtering system in the bedrooms of children with asthma.
The average cost of the comprehensive GHHI Asthma Reduction program health and energy intervention is $5,500–10,000 for higher level interventions; the program is supported by grants, and there is no cost to participants.
Program data and evaluation staff conduct health surveys with participants both before and after interventions (at 3-, 6-, 9-, and 12-month intervals) to ascertain health, school attendance, work attendance, and other family stability outcomes. GHHI uses WegoWise software for 12-month pre- and postutility data analysis to measure energy consumption and any energy cost reductions. GHHI program data show that participating program households are saving an average of $306 annually on utility bills postintervention, in addition to medical cost savings.
Postintervention health outcomes indicate that the participants with asthma are experiencing fewer emergency room visits, hospital admissions, and missed school days, while their parents are experiencing fewer missed workdays. Further, caregivers of children with asthma have reported a 74% reduction in uncontrolled episodes. Program data and evaluation staff have documented a reduction in childhood asthma-related hospitalizations for program participants of 66% and a 62% increase in asthma-related perfect school attendance. As part of the program’s Healthy Homes Technical Study, funded by HUD, GHHI is also capturing pre- and postintervention school attendance data and Medicaid cost data.
Recommendations and Conclusions
The case studies cited above highlight some of the ways that programs can assess the health effects of energy efficiency interventions; however, the limited data derived from these studies make it challenging to identify a standard set of methods or best practices. Nine programs conducted some form of preintervention environmental health assessment to establish a baseline against which outcomes could be compared. More work is needed to identify common elements of these approaches and to determine what information is needed to accurately assess outcomes.
Some of the programs tracking health outcomes have formed collaborative relationships with local health departments or medical centers that can provide the data and expertise needed to track and report these outcomes accurately.
While experience in tracking and reporting on the health benefits of energy efficiency programs is limited, progress so far can help those programs to quantify the additional value of preventing health harms and improving occupants’ health. This can help expand sources of program funding by demonstrating greater benefits for each dollar invested in utility-funded programs. Potentially, it could also attract health-focused funders such as hospitals and other health care providers seeking to reduce hospitalizations and improve community health. This article provides only a glimpse into the current state of practice, and perhaps the most important finding is that much more work is needed to help programs succeed in both saving energy and protecting people’s health.
Earn CEUs
Earning CEUs on the BPA Journal is a member-exclusive benefit. Please log in to complete the quiz and earn them or join as a member today.




